Tibial Tubercle Osteotomy (TTO), also referred to as Tibial Tubercle Transfer (TTT), is a technique used in the treatment of patellofemoral disorders, most commonly correcting patellofemoral malalignment in the setting of patellar instability.
The technique involves cutting the tibial tubercle and shifting it in the desired direction and magnitude in order to realign the extensor mechanism. In addition to malalignment, TTO is also performed in the setting of abnormal patellar height (patellar alta) and to offload symptomatic focal chondral lesions of the patella or trochlea. The most commonly performed TTO technique, as originally described by Fulkerson, involves an oblique anteromedialization (AMZ) osteotomy. Other techniques have more limited applications today and include straight anteriorization8 of the tibial tubercle to unload the patellar cartilage and straight medialization6 of the tubercle to realign the extensor mechanism. Furthermore, distalization to correct patella alta and/or offload inferior pole chondral lesions has received increased attention in contemporary patellofemoral surgery. Multiple physical examination tests and imaging parameters, as well as (physiologic) age, activity level, symptom burden, prior treatments, and alternatives are carefully weighed when indicating TTO. Concurrent surgeries are commonly performed including arthroscopy, chondroplasty, cartilage restoration procedures, medial patellofemoral ligament reconstruction, and lateral reticular lengthening. Multiple studies have shown successful outcomes with the AMZ TTO for varying patellofemoral pathology.1,2,3 Two recent systematic reviews further support the benefits of AMZ TTO with significant improvements in multiple clinical outcome scores and patient-reported outcomes.4,5 This article will highlight considerations related to TTO for the orthopedic sports medicine surgeon.
Evolution of the Tibial Tubercle Osteotomy:
TTO was described by Roux in 1888 and later popularized by Elsmlie and Trillat to correct patellofemoral instability by medializing the tibial tubercle.6 Maquet described a technique for tibial tubercle anteriorization in 1963 to offload the patellofemoral articulation in the setting of arthritis.7,8 This iteration of the procedure has lost favor due to soft tissue and wound complications, however more contemporary techniques have been developed.9 The AMZ TTO introduced by Fulkerson in 1983 is a versatile procedure in which the oblique osteotomy can be performed at different angles to titrate the desired shift in sagittal and coronal planes.10
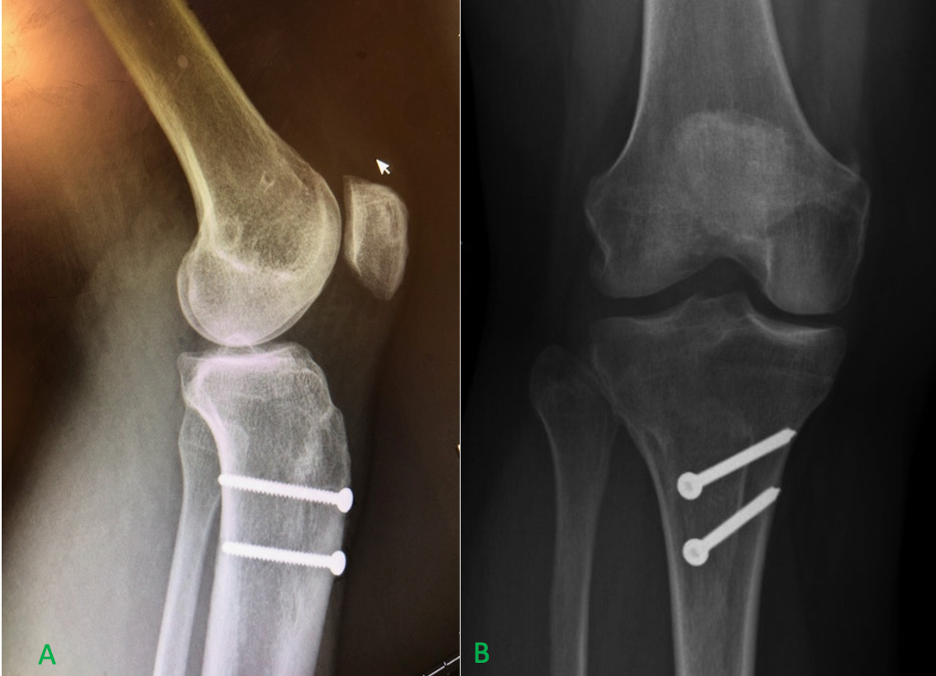
Long-term follow-up for Fulkerson’s AMZ has demonstrated improved efficacy and reduced complications compared to earlier osteotomy techniques.11 Postoperative radiographs of an AMZ TTO can be seen in Figure 1. While straight medialization may continue to be used in cases of patellar instability without chondral pathology, the AMZ has become the workhorse procedure.12 There have been numerous modifications to the original AMZ technique described by Fulkerson in the form of proprietary cutting jigs to help simplify the procedure as well increase accuracy and reproducibility. The TTO technique has continued to evolve with the development of the multidirectional tibial tubercle transfer system (MD3TTM) by Merchant in 2016 which involves cutting triangular shaped wedges which can be transposed in difference directions to allow for medial, anterior, distal, proximal and AMZ transfers.13 In addition, computed tomography (CT) based plans for individualized osteotomies with patient specific fixation are poised to offer precision and detailed planning for complex cases.14
Patient Evaluation
Indications for TTO include correction of patellofemoral maltracking, abnormal patellar height, recurrent patellar instability, and offloading articular cartilage pathology including focal articular cartilage lesions, more diffuse patellofemoral arthrosis, and less commonly recalcitrant patellofemoral pain related to lateral overload.15 Considerations for planning a TTO and concomitant procedures include assessment of the bony anatomy, particularly limb and extensor mechanism alignment, patellar height and tilt, and trochlear dysplasia. The status of the cartilage, whether a focal defect or compartmental disease, is also important and may need to be addressed with chondroplasty or a cartilage restoration procedure in addition to an unloading osteotomy. The soft tissue is also frequently addressed in the form of medial patellofemoral ligament (MPFL) or medial quadriceps tendon femoral ligament (MQTFL) reconstruction for instability with possible release or lengthening of the lateral retinaculum.
TTO for Patellar Instability
Patellar instability is the most common indication for TTO. Medialization decreases lateralizing forces while anteriorization offloads the patellofemoral articulation. Distalization may also be used for correction of patella alta to improve osseous constraint by allowing the patella to engage the trochlea at a lower knee flexion angle.16 The AMZ allows for realignment of the tubercle in multiple planes, with different angles of the oblique cut allowing for different ratios of coronal and sagittal shift. In patients with a lateralized tubercle and instability or lateral facet overload, the AMZ can improve patellar tracking while also shifting patellofemoral contact stress medially and proximally.11,17
Tibial Tubercle to Trochlear Groove Distance (TT-TG)
The tibial tubercle to trochlear groove (TT-TG) distance is frequently used as an imaging parameter for lateralization of the extensor mechanism and thus to quantify the lateral force vector on the patella; increased TT-TG is associated with patellofemoral instability. Values above 15mm are considered abnormal with values above 20mm considered pathologic.
Tibial Tubercle to Posterior Cruciate Ligament Distance (TT-PCL)
The tibial tubercle to posterior cruciate ligament distance (TT-PCL) is an alternative measure proposed to avoid potential variability in measurements due to rotation of the tibia on the femur at different knee flexion angles. It does not rely on identifying the center of the trochlea, which may be difficult in the setting of trochlear dysplasia. A normal TT-PCL is less than 24mm.18
Caton-Deschamps Index (CDI)
Patella alta can contribute to patellar instability as engagement of the patella within the trochlea occurs later in flexion, thus reducing the bony constraint of the patellofemoral joint and predisposing the patient to patellar instability.19 The Caton-Deschamps index is one of several methods used to measure patellar height, and utilizes the articular surface of the patella and its ratio with the distance from the tibial plateau. A normal ratio range is from 0.6 to 1.3, with values lower and higher indicating patella baja and alta, respectively. When distalization is performed in TTO, the goal CDI is 1.1-1.2.15
Patellotrochlear index
Another method of measuring patellofemoral sagittal plane alignment includes the patellotrochlear index introduced by Biedert and the modification of this by Dejour to describe the sagittal patellofemoral engagement index.20,21 These indices measure the ratio between the length of the patellar cartilage and the corresponding trochlear cartilage to determine patellar height and engagement of the patella and trochlea. The normal patellotrochlear index values range from 0.18 to 0.8, with values lower and higher indicating patella alta and baja, respectively.20
TTO for Articular Cartilage Disease
TTO may also be performed for patellofemoral arthritis or in conjunction with cartilage restoration procedures.22 This is achieved by anteriorizing the tubercle and thus reducing the compressive forces across the joint. Patient outcomes after cartilage restoration procedures have been shown to be improved with the addition of an unloading TTO.23,24 Patients with distal or lateral patellar chondral lesions undergoing TTO have excellent results, with less predictable outcomes for patients with medial, proximal or central trochlear lesions.25 Straight anteriorization is not used for patellar instability. It is important to note there are skin and wound complications associated with excessive anteriorization due to the limited soft tissue envelope at the level of the tubercle, which has contributed to such procedures becoming less popular.9 However, when indicated and with careful technique, anteriorization remains an important method for treatment of patellofemoral articular cartilage pathology.
Technical Considerations

Essential to successful TTO surgery is correction of the underlying pathoanatomy based on preoperative planning and confirmed by intra-operative assessments. Ultimately, that means normalizing TT-TG, TT-PCL, CDI, patellotrochlear index, or other measures that were the basis for indicating surgery. The details of the multiple described TTO techniques and their variations are beyond the scope of this overview, however basic considerations include free-hand versus instrument guided cuts, whether the distal aspect of the tubercle shingle is detached or left intact, the shape of the cut, and the order of operations when performed with concomitant ligament or cartilage restoration procedures. In addition, there are multiple options for fixation including solid versus cannulated headed screws, headless compression screws, and plate and screw constructs such as the Bristol technique.26
Thorough evaluation of the patient’s concurrent pathology is needed to determine adjunctive procedures. Generally, with instability cases, MPFL reconstruction is commonly performed with TTO, and occasionally a lateral lengthening or release may be added. Diagnostic arthroscopy is helpful to evaluate intra-articular pathology and visualize patellar tracking, and allows for chondroplasty and/or loose body removal if indicated. Cartilage restoration techniques such as osteochondral allograft (OCA) or matrix-induced autologous chondrocyte implantation (MACI) may be added for focal cartilage defects. Figure 2 demonstrates a postoperative radiograph of a patellar OCA and figure 3 demonstrates an intraoperative image of a patellar MACI, both performed in conjunction with a TTO.

In the setting of recurrent patellar instability with a lateralized tubercle and resultant chondral injury, it may be necessary to perform MPFL reconstruction, TTO, and cartilage restoration concurrently, however, diligent evaluation of each patient’s pathoanatomy should guide individualized treatment plans. In the future, it is likely that patient specific advanced imaging-based plans may help enhance the precision of these procedures.
Postoperative Rehabilitation
Standard postoperative rehabilitation after TTO has typically included a period of nonweightbearing with bracing in extension to reduce the risk of tibial fracture or fixation failure. After 6-8 weeks, weightbearing is advanced and ROM and strengthening exercises are implemented3. More recently, accelerated rehabilitation protocols are gaining favor as they have been demonstrated to result in improvements in strength, ROM, and pain in procedures such as TKA and ACL reconstruction. A recent study found no increased incidence of postoperative complications with an accelerated rehab protocol27. The senior author (TBS) favors an accelerated rehabilitation allowing early weight bearing with a brace locked in extension and two crutches and motion as tolerated for instability cases. Postoperative rehabilitation parameters in cases with concurrent articular cartilage restoration are generally dictated by the articular cartilage procedure.
Outcomes
Studies following TTO have consistently reported successful outcomes for a number of patellofemoral conditions including malalignment, instability, and chondral disease.1,2,3,4,5 Recent data has supported that the addition of TTO to an MPFL reconstruction reduces revision rates versus isolated MPFL reconstruction.28 While outcomes of well indicated TTOs are generally quite favorable, complications can occur, with more serious complications being less common. These include recurrent instability, tibial tubercle or proximal tibia fractures, delayed union or nonunion of the osteotomy, wound complications or infection, neurovascular injury, and painful hardware. There is a roughly 20% reoperation rate with about 16% being for painful hardware removal4,29. Painful hardware has been found to be significantly more common with 4.5mm screws versus 3.5mm screws29. There is a 3-4% incidence of DVT.29,30 Delayed union is more common with distalization, likely due to requiring complete detachment of the distal tuberosity during the osteotomy, however clinical nonunion is not common.29 There are low (<1%) rates of conversion to HTO, PFA, or TKA. Revision TTO has been reported in 1.5% of cases.4 The senior authors’ (TBS, EIF, EEV) experience has been that using headless screws decreases the incidence of symptomatic hardware and subsequent surgery for removal compared to countersunk large fragment screws.
New Techniques and Emerging Technology

A newer technique, the multi-directional tibial tubercle transfer system (MD3TTM) has been introduced in recent years. This system uses a proprietary cutting guide to create primary and secondary wedges of bone and transposes the wedges in order to transfer the tubercle in the desired direction and magnitude. It allows for independent adjustments of medial, anterior, proximal, and distal transfers, as well as the ability to perform a combined transfer in the sagittal and coronal planes. Unlike the AMZ technique, this system creates a triangular primary osteotomy with corresponding triangular shaped osteotomy bed with intact medial and lateral cortices providing inherent bony stability (Figure 4). The proposed benefits of this system include precision and flexibility of the transfer, safety and simplicity of the cut, decreased soft tissue disruption, and potentially allowing for accelerated recovery and rehabilitation due to secure fixation and inherent osteotomy stability.13

Another example of emerging technology is CT-based patient specific instrumentation (Figure 5). Such technology has been utilized for coronal plane osteotomies and is most commonly utilized for robotic assisted knee arthroplasty.31 While utilization of CT based planning and patient specific instrumentation is still nascent with regard to patellofemoral pathology, we believe this technology has great potential for improving the precision and reproducibility of TTO. Moreover, for challenging cases such as revision surgery or severe trochlear dysplasia cases, 3D modeling may help surgeons better understand complex patellofemoral anatomy, so we believe this technology will likely become an important tool in patellofemoral surgery.14
Other Considerations
While TTO is a powerful treatment in the setting of patellar instability, it is not all-encompassing. Beyond the scope of this article are several other procedures which may be indicated depending on the underlying pathology. Trochlear dysplasia diminishes the bony stability of the patellofemoral joint and frequently leads to recurrent patellar instability.32 Trochleoplasty is a procedure which aims to restore bony stability to the patellofemoral joint, often performed with other stabilizing procedures including TTO, however reported success rates are mixed and more research is needed on long term outcomes.33
While the TT-TG provides a local assessment of coronal alignment, there are other forms of malalignment which can be responsible for patellar instability. Genu valgum in the coronal plane, as well as increased femoral anteversion or internal torsion and external tibial torsion in the axial plane all contribute to an increased Q angle and subsequent instability. Genu valgum is addressed with a distal femoral varus-producing osteotomy, while femoral and tibial torsion can be addressed with rotational osteotomies.34
There are a range of cartilage procedures which may be performed including debridement/chondroplasty, osteochondral fixation, OCA, MACI, and more. The type of procedure depends on the injury characteristics, including size, acuity, bony involvement, and, in the case of chondral or osteochondral fracture, the amenability of the fragment(s) to repair.
Summary
TTO is a versatile procedure in the treatment of patellofemoral instability, malalignment, and patellofemoral articular cartilage pathology, with favorable outcomes. The direction and magnitude of transfer can be tailored in various ways to treat a corresponding variety of pathology. It is common for TTO to be utilized in conjunction with other procedures depending on each patient’s anatomy and underlying disease, and a thoughtful approach in evaluating each individual case to determine the indicated procedures is critical. Techniques continue to evolve, with newer osteotomy guides as well as the use of CT imaging, 3D modeling, and patient specific instrumentation becoming increasingly available to assist surgeons in more complex cases.
References
- Farr J, Schepsis A, Cole B, Fulkerson J, Lewis P. Anteromedialization: review and technique. J Knee Surg. 2007;20(2):120-128.
- Pritsch T, Haim A, Arbel R, Snir N, Shasha N, Dekel S. Tailored tibial tubercle transfer for patellofemoral malalignment: analysis of clinical outcomes. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):994- 1002.
- Sherman SL, Erickson BJ, Cvetanovich GL, Chalmers PN, Farr J 2nd, Bach BR Jr, Cole BJ. Tibial Tuberosity Osteotomy: Indications, Techniques, and Outcomes. Am J Sports Med. 2014 Aug;42(8):2006-17. Doi: 10.1177/0363546513507423. Epub 2013 Nov 6. PMID: 24197613
- Saltzman BM, Rao A, Erickson BJ, Cvetanovich GL, Levy D, Bach BR Jr, Cole BJ. A Systematic Review of 21 Tibial Tubercle Osteotomy Studies and More Than 1000 Knees: Indications, Clinical Outcomes, Complications, and Reoperations. Am J Orthop (Belle Mead NJ). 2017 Nov/Dec;46(6):E396-E407. PMID: 29309452.
- Rosso F, Rossi R, Cottino U, Bonasia DE. Tibial tubercle osteotomy for patellofemoral malalignment and chondral disease provided good outcomes: A systematic review. J ISAKOS. 2022 Apr;7(2):78-86. Doi: 10.1016/j.jisako.2021.10.002. Epub 2021 Nov 17. PMID: 35546438.
- Trillat A., Dejour H., Couette A. Diagnostic et traitement des subluxations récidivantes de la rotule. Rev Chir Orthop Reparatrice Appar Mot. 1964;50:813–824.
- Maquet P. A biomechanical treatment of femoro- patellar arthrosis: Advancement of the patellar tendon. Rev Rhum Mal Osteoartic. 1963;30:779-83.
- Maquet P. Advancement of the tibial tuberosity. Clin Orthop Relat Res. 1976;115:225-230.
- Bessette GC, Hunter RE. The Maquet procedure: a retrospective review. Clin Orthop Relat Res. 1988;232:159-167.
- Fulkerson J.P. Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res. 1983;177:176–181
- Buuck D, Fulkerson J. Anteromedialization of the tibial tubercle: a 4-12 year follow up. Operative Techniques in Sports Medicine. 2000;8:131-137.
- Colvin AC, West RV. Patellar instability. J Bone Joint Surg Am. 2008;90(12):2751-2762.
- Sarin VK, Camisa W, Leasure JM, Merchant AC. Multidirectional Tibial Tubercle Transfer Technique: Rationale and Biomechanical Investigation. J Surg Orthop Adv. 2016 Fall;25(3):157-164. PMID: 27791972.
- Beitler BG, Yu KE, Wang A, Frumberg DB, Tommasini SM, Wiznia DH, Cooperman DR, Lattanza LL, Fulkerson JP. Three-Dimensional Printing of the Patellofemoral Joints of Patellar Instability Patients. Arthrosc Tech. 2023 Feb 27;12(3):e401-e406. Doi: 10.1016/j.eats.2022.11.023. PMID: 37013007; PMCID: PMC10066413.
- Middleton KK, Gruber S, Shubin Stein BE. Why and Where to Move the Tibial Tubercle: Indications and Techniques for Tibial Tubercle Osteotomy. Sports Med Arthrosc Rev. 2019 Dec;27(4):154-160. doi: 10.1097/JSA.0000000000000270. PMID: 31688534.
- Mayer C, Magnussen RA, Servien E, Demey G, Jacobi M, Neyret P, Lustig S. Patellar tendon tenodesis in association with tibial tubercle distalization for the treatment of episodic patellar dislocation with patella alta. Am J Sports Med. 2012 Feb;40(2):346-51. doi: 10.1177/0363546511427117. Epub 2011 Nov 22. PMID: 22109545.
- Lamplot JD, Jahandar A, Meyers KN, Gomoll AH, Maher SA, Strickland SM. Anteromedialization Tibial Tubercle Osteotomy Improves Patellar Contact Forces: A Cadaveric Model of Patellofemoral Dysplasia. Am J Sports Med. 2023 Feb;51(2):453-460. doi: 10.1177/03635465221138287. Epub 2022 Dec 1. PMID: 36453729.
- Seitlinger G, Scheurecker G, Hogler R, Labey L, Innocenti B, Hofmann S. Tibial tubercle-posterior cruciate ligament distance: a new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am J Sports Med. 2012;40(5):1119-1125.
- Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19-26.
- Biedert RM, Albrecht S. The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthrosc. 2006 Aug;14(8):707-12. doi: 10.1007/s00167-005-0015-4. Epub 2006 Feb 23. PMID: 16496126.
- Dejour D, Ferrua P, Ntagiopoulos PG, Radier C, Hulet C, Rémy F, Chouteau J, Chotel F, Boisrenoult P, Sebilo A, Guilbert S, Bertin D, Ehkirch FP, Chassaing V; French Arthroscopy Society (SFA). The introduction of a new MRI index to evaluate sagittal patellofemoral engagement. Orthop Traumatol Surg Res. 2013 Dec;99(8 Suppl):S391-8. doi:
10.1016/j.otsr.2013.10.008. Epub 2013 Nov 15. PMID: 24246663. - Farr J. Autologous chondrocyte implantation improves patellofemoral cartilage treatment outcomes. Clin Orthop Relat Res. 2007;463:187-194.
- Trinh TQ, Harris JD, Siston RA, Flanigan DC. Improved outcomes with combined autologous chondrocyte implantation and patellofemoral osteotomy versus isolated autologous chondrocyte implantation. Arthroscopy. 2013;29(3):566-574
- Gallo RA, Feeley BT. Cartilage defects of the femoral trochlea. Knee Surg Sports Traumatol Arthrosc. 2009;17(11):1316-1325.
- Pidoriano AJ, Weinstein RN, Buuck DA, Fulkerson JP. Correlation of patellar articular lesions with results from anteromedial tibial tubercle transfer. Am J Sports Med. 1997;25(4):533-537.
- Stevens JM, Barton SB, Alexander M, Eldridge JD, Clark D. Plate and screw fixation of arthroscopically assisted tibial tuberosity osteotomy: technique and results. Eur J Orthop Surg Traumatol. 2020 Jan;30(1):139-145. doi: 10.1007/s00590-019-02536-x. Epub 2019 Aug 28. PMID: 31456034.
- Morgan C, Bell RM, Burland JP, Kriscenski D, Ilinski A, Cote MP, Edgar CM. Effectiveness of an Accelerated Rehabilitation Protocol After Tibial Tubercle Osteotomy. Orthop J Sports Med. 2022 Nov 29;10(11):23259671221133105. doi: 10.1177/23259671221133105. PMID: 36479459; PMCID: PMC9720819.
- Ryan PC, Ross BJ, Stamm MA, Sherman WF, Heard WMR, Mulcahey MK. Concomitant Tibial Tubercle Osteotomy Reduces the Risk of Revision Surgery After Medial Patellofemoral Ligament Reconstruction for the Treatment of Patellar Instability. Arthroscopy. 2023 Feb 18:S0749-8063(23)00170-6. doi: 10.1016/j.arthro.2023.02.006. Epub ahead of print. PMID: 36804459.
- Johnson AA, Wolfe EL, Mintz DN, Demehri S, Shubin Stein BE, Cosgarea AJ. Complications After Tibial Tuberosity Osteotomy: Association With Screw Size and Concomitant Distalization. Orthop J Sports Med. 2018 Oct 19;6(10):2325967118803614. doi: 10.1177/2325967118803614. PMID: 30364433; PMCID: PMC6196632.
- Tanaka MJ, Munch JL, Slater AJ, Nguyen JT, Shubin Stein BE. Incidence of deep venous thrombosis after tibial tubercle osteotomy: a single case series study. Orthop J Sports Med. 2014;2(8): 2325967114544457.
- Sherman S, Ray T, Pullen M. Knee Osteotomy for the Tibiofemoral Joint. Sports Medicine Update. Issue 2, 2021.
- Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med 2013;41:575–81.
- LaPrade RF, Cram TR, James EW, Rasmussen MT. Trochlear dysplasia and the role of trochleoplasty. Clin Sports Med. 2014 Jul;33(3):531-45. doi: 10.1016/j.csm.2014.03.005. Epub 2014 May 24. PMID: 24993414.
- Taylor J. Reif, Tyler J. Humphrey, Austin T. Fragomen. Osteotomies About the Knee: Managing Rotational Deformities. Operative Techniques in Sports Medicine, Volume 30, Issue 3, 2022